Overview
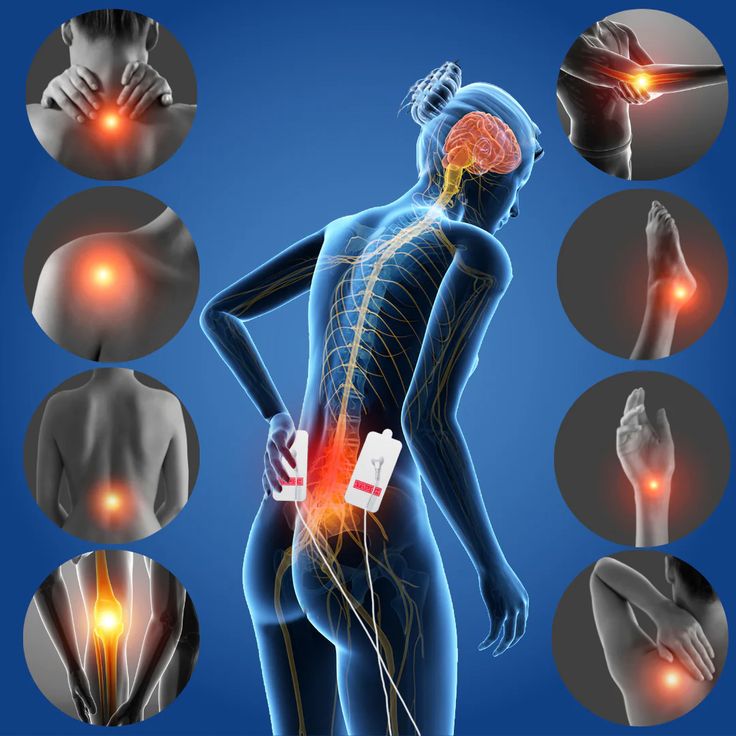
In addition to treating the physical symptoms of pain, holistic methods to pain management treatment also address the mental, emotional, and spiritual dimensions of health and wellbeing. These holistic approaches acknowledge the relationship between the mind, body, and spirit in fostering resilience and general well-being. In order to better understand how incorporating mind-body-spirit activities can improve pain alleviation and quality of life, we will examine a variety of holistic approaches to pain treatment in this article.
Comprehending Complementary Medical Care
Mind-Body Connection: A key component of integrative pain treatment is the mind-body connection. Our perception and reaction to pain can be influenced by our ideas, feelings, and beliefs. Holistic treatments seek to lessen the intensity of pain and enhance coping mechanisms by addressing psychological variables such stress, worry, and depression.
Spiritual Wellness: Providing a feeling of direction, community, and resilience, spirituality is important for holistic recovery. Techniques like mindfulness, meditation, prayer, and guided imagery can improve overall pain treatment results while also promoting spiritual well-being.
Pain Reduction Through Mindful Meditation
Practices of Mindfulness: Developing a judgment-free present-moment awareness is a component of mindfulness meditation. Because it fosters relaxation, lowers stress levels, and increases acceptance of pain, it can be an effective strategy for controlling pain. Mindfulness meditation is a fundamental part of pain treatment in many mindfulness-based stress reduction (MBSR) programs.
Advantages of Mindfulness Meditation:
Research indicates that consistent mindfulness meditation practice can result in notable decreases in pain intensity, better coping mechanisms for pain, and increased general wellbeing. Through the practice of training the mind to remain detached from ideas and sensations, people can become more resilient to pain.
Using Yoga Therapy to Treat Pain
Yoga Principles: Yoga is a holistic discipline that incorporates breathing exercises (pranayama), physical postures (asanas), and meditation methods. These ideas are modified in yoga therapy to meet particular health issues, such as chronic pain syndromes.
Advantages of Yoga for Pain Relief:
The main goals of yoga therapy for pain relief include mild stretching, strengthening exercises, and relaxation methods. It can ease pain and boost quality of life by promoting stress reduction, enhancing body awareness, reducing muscle tension, and improving flexibility.
Nutrition-Based Pain Management Strategies
Anti-Inflammatory Diet: Nutrition is an important component of comprehensive pain treatment, especially when it comes to treating inflammatory diseases. Pain can be lessened and inflammation can be decreased with an anti-inflammatory diet high in fruits, vegetables, whole grains, lean meats, and healthy fats like omega-3 fatty acids.
Supplements for Pain Relief:
Some supplements include anti-inflammatory and analgesic qualities that may support holistic pain treatment. Examples of these are vitamin D, fish oil, ginger, and turmeric (curcumin). Before beginning any new supplement regimen, it is imperative to speak with a healthcare professional because some supplements may have negative effects or interfere with prescription drugs.
Complementary Bodywork Practices
Massage Therapy: Offering advantages for the body, mind, and soul, massage therapy is a well-liked integrated technique to pain treatment. Numerous massage techniques, including deep tissue, Swedish, and myofascial release massages, can soothe pain, enhance circulation, ease tense muscles, and encourage relaxation.
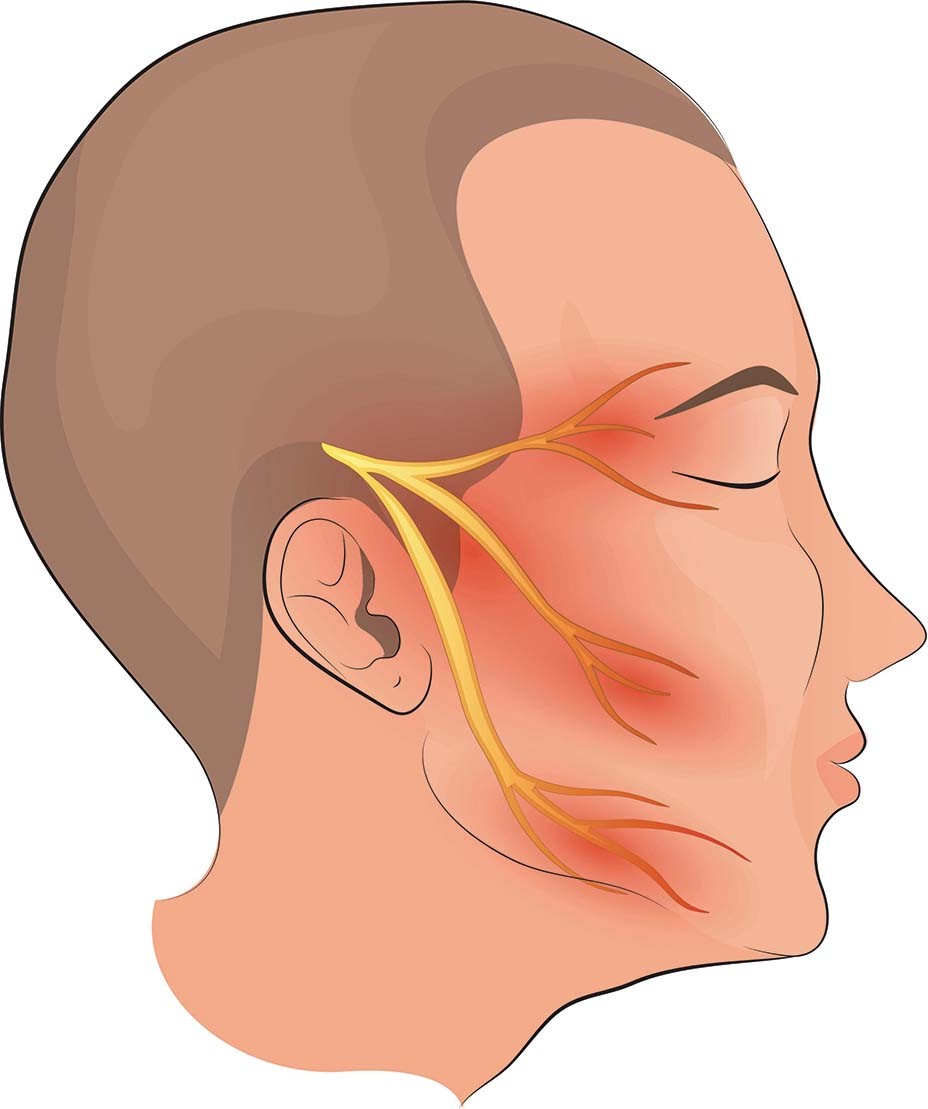
Acupuncture and Acupressure:
These traditional Chinese medicine techniques work by applying pressure to certain meridian sites in order to let the body’s energy flow and equilibrium return. Back pain, arthritis, and fibromyalgia are a few chronic pain disorders that these therapies can help with.
Mental and Emotional Assistance
Counseling & Therapy:
A comprehensive approach to pain treatment must include both emotional and psychological support. Psychotherapy, cognitive-behavioral therapy (CBT), and counseling can assist people in addressing underlying emotional problems, creating coping mechanisms, and strengthening their ability to withstand discomfort.
Techniques for Reducing Stress:
The foundation of an all-encompassing approach to pain treatment is stress management. Methods that lower stress, encourage relaxation, and improve general well-being include progressive muscle relaxation, guided imagery, biofeedback, and deep breathing exercises.
In summary
In order to promote overall health and well-being, holistic approaches to pain reduction acknowledge the interdependence of mind, body, and spirit. Through the integration of integrative bodywork therapies, nutritional methods, emotional support, and mindful meditation, people can receive complete pain management that improves quality of life and targets the underlying causes of pain. Working together with patients to create individualized, holistic pain treatment programs that fit their objectives, values, and preferences is crucial for healthcare professionals. The integration of the mind, body, and spirit can result in a pain alleviation treatment that is both efficient and long-lasting.